According to the World Health Organisation, “Blood pressure is the force exerted by circulating blood against the walls of the body’s arteries, the major blood vessels in the body. Hypertension is when blood pressure is too high.”
Once a woman is pregnant, she might develop hypertension. It can influence the body in unforeseen ways in comparison to the general high blood pressure.
This might put both mother and child at high risk for complications. If the mother initially develops it when she is pregnant, it is called gestational hypertension or pregnancy-instigated hypertension.
Gestational hypertension happens when the blood pressure ascends in the second half of the pregnancy. Blood pressure is the force of blood pushing against artery walls through veins.
When this pressure increases more than 140/90 mm Hg, physicians consider the pulse of a mother to be high.
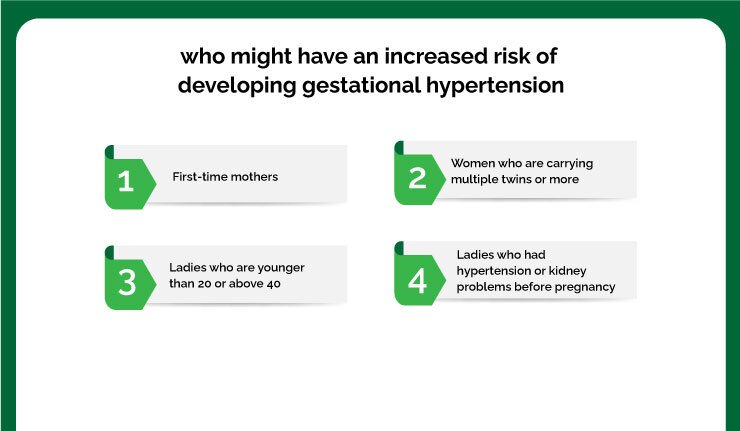
The women who might have an increased risk of developing gestational hypertension are
- First-time mothers
- Women who are carrying multiple twins or more
- Ladies who are younger than 20 or above 40
- Ladies who had hypertension or kidney problems before pregnancy
Table of Contents
ToggleDiagnosis
At every prenatal check-up, the primary physician will check the pulse to keep a watch for gestational hypertension.
The doctor may request blood tests, do an ultrasound scan to check the fetus’s development, and utilize a Doppler Scan to gauge bloodstream efficiency to the placenta.
Treatment
Treatment relies upon the fact that the mother is near her due date, and the infant is entirely developed, then the gynecologist might want to deliver the infant as quickly as time permits.
If the mother has mild hypertension and her infant is not completely evolved, then her primary physician will most likely suggest the following
- Taking rest by lying on to her left side which will help keep the baby’s weight off the major blood vessels.
- Increase prenatal check-ups.
- Consume less salt.
- Drink eight glasses of water every day.
- If the mother tends to have acute gestational hypertension, then the primary physician may attempt to treat her with blood pressure related medicines for the safe delivery of the baby.
Risk factors
Hypertension at the time of pregnancy poses various risks, including:
1. Decreased blood flow to the placenta
If the placenta doesn’t get enough blood, the baby might receive less oxygen and fewer nutrients. It can cause slow growth (intrauterine growth restriction), low birth weight, or premature birth.
2. Placental abruption
Preeclampsia increases the mother’s risk of developing this condition when the placenta separates from the inner wall of her uterus before delivery. Severe abruption can cause heavy bleeding, which might be life-threatening for both the mother and baby.
3. Intrauterine growth restriction
Gestational hypertension might lead to slowed or decreased growth of the baby (intrauterine growth restriction).
4. Injury to the other organs
Poorly controlled hypertension may damage the mother’s brain, heart, lungs, kidneys, liver, and other major organs. In severe cases, it may be life-threatening.
5. Premature delivery
Sometimes, early delivery is required to stop potentially life-threatening complications after high force per unit area during pregnancy.
6. Future disabilities
Having preeclampsia might increase the risk of future heart and vessel (cardiovascular) disease. The mother’s risk of future disabilities is higher if she has had preeclampsia quite once or has had a premature birth due to hypertension during pregnancy.
Preventive methods
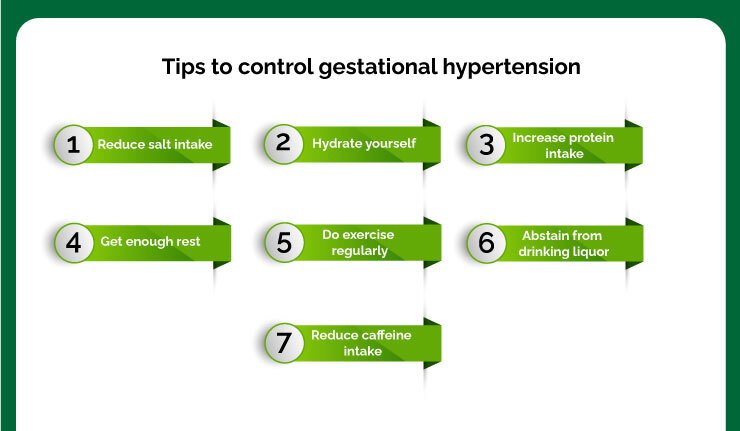
As of now, there is no precise method to control hypertension though some contributing elements to hypertension can be controlled, while others can’t. Adhere to the primary physician’s directions about eating routine and exercise.
A few different ways that can help control gestational hypertension are by incorporating the following:
- Utilize salt as needed only for taste.
- Drink, at any rate, eight glasses of water a day.
- The level of protein intake must be increased, and decline the quantity of fried and junk food.
- Get enough rest.
- Do exercise regularly.
- Abstain from drinking liquor.
- Maintain a strategic distance from refreshments containing caffeine.
- The primary physician may also propose the mother to take the medication and extra enhancements.
To Conclude
(Hypertension) during pregnancy commonly disappears after the child is delivered yet expands the danger of hypertension and coronary illness later on.
Ladies who had ceaseless hypertension before pregnancy will generally have the condition after delivery. Now and then, blood pressure can stay high after childbirth, requiring treatment with medication.
The primary physician will work with the mother after her pregnancy to deal with the blood pressure related issues. It is crucial for pregnant women to know the importance of prenatal screening for a safe pregnancy.
All the information provided by Jammi Scans through its video, blog series is strictly for informational purposes only and all content, including text, graphics, video, images and information, contained on or available through this web site are only general information about gynecology, obstetric ultrasound scan services, practices and standards and the same is intended for information purposes only.
Any video, audio or text content is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. The information provided by Jammi Scans should not be used to self-diagnose or self-treat any health condition. Always seek the advice of your physician or other qualified health provider on any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of some information/inference you may have gathered from any video, audio or text content published by Jammi Scans.
The medical information, on any platform (digital or print), created by Jammi Scans is provided “as is” without any representations or warranties, express or implied. Jammi Scans shall not be responsible or liable for the use of any advice or information that you may obtain through this web site as a substitute for professional medical advice, diagnosis or treatment.