Table of Contents
ToggleIntroduction
Have you often heard that hormones play an important role in shaping the human body? Yes, you have heard it right. Post puberty, the rush of hormones is high, and usually, problems arise when there is an imbalance in them.
Polycystic Ovary Syndrome (PCOS) is one such ailment that occurs due to hormonal disparities. The goal of this guide is to help the readers understand what PCOS is, its causes, signs and symptoms, the fertility issues it brings up, diagnosis, early interventions, and the treatment available.
What is Polycystic Ovary Syndrome (PCOS)?
A very simple way to understand PCOS is that it’s an endocrine system disorder. The endocrine system is the glandular factory that produces necessary hormones to balance out reproduction, metabolism, sexual activities, sleep, and mood.
The four types of PCOS are

1. Insulin-resistant PCOS:
Most common PCOS type, is due to the result of high levels of insulin in the body. Insulin-resistant PCOS is also referred to as metabolic syndrome or pre-diabetes.
2. Post-pill PCOS:
This type of PCOS is often temporary, and arises due to recent oral contraception. It heals by itself with the right amount of lifestyle, diet, and nutritional intake.
3. Inflammatory PCOS
is when chronic inflammation in the body influences higher androgen levels.
4. Adrenal PCOS:
Neither of the above, the Adrenal PCOS arises due to the body’s response to stress.
The root causes of PCOS - hormonal imbalance
Even though the exact cause of PCOS is still unknown, from what the researchers have proven, PCOS results in hormonal imbalances, obstructing ovulation—the unique way by which the body produces and releases eggs from the ovary.
The endocrine disorder disrupts hormonal function and is often characterized by three main elements;
(1) Chronic Anovulation:
It is quite natural for women with PCOS to have unsuitable production of FSH (follicle-stimulating hormone) and LH (Luteinizing Hormone), due to which they confront limited follicular development—a state when small sac-like structures (cysts) are formed within the ovaries, which obstructs or limits the egg release. When there is a limit in the egg development, it clinically may result in Ovulatory Dysfunctions like;
- Irregular sporadic ovulation: indication when there is irregular ovulation
- Anovulation: when ovulation is entirely absent
Ovulatory dysfunction is mainly responsible for causing fertility issues in women. When anovulation prolongs, the endometrial tissue lining in the uterus gets thickened, leading to irregular periods.
(2) Increase in Androgen Levels:
The tiny sac-like cysts trigger the production of excess “androgens”. Androgens being the male dominating hormones, causes more problems with a woman’s menstrual cycle.
The complication of hyperandrogenism could also lead to high levels of blood cholesterol.
(3) Insulin Resistance:
One of the root causes of PCOS, insulin resistance occurs when the pancreas needs to pump out more and more insulin in response to high blood sugar levels. Insulins are responsible for lowering your blood sugar by storing the glucose in cells.
The cells become resistant to the constant insulin and need additional signals to lower the blood sugar. When this resistance continues for a while, there occurs high insulin and high blood sugar. High insulin levels can signal the ovaries to produce more testosterone.
This is another reason why generally women with PCOS have excess androgen symptoms including excessive hair growth on the face, abdomen.
What are the symptoms of PCOS?
The first few signs which indicate that you need a diagnosis for PCOS is when you have two or more of the following symptoms;
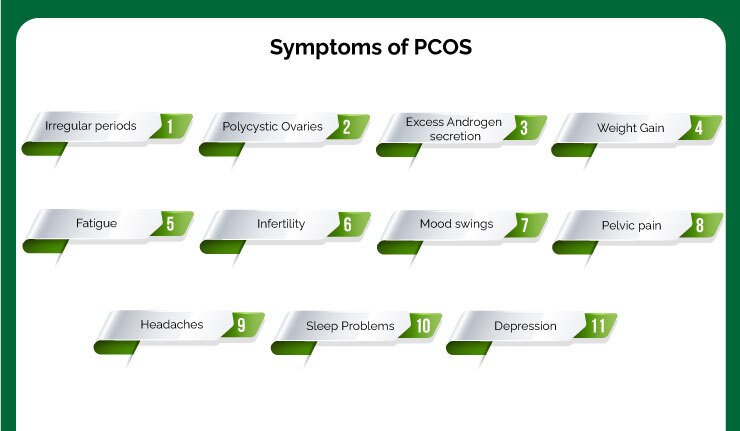
(1) Irregular periods:
Irregular or missed periods that usually occur due to the failure of ovulation are the first common sign of PCOS. While the normal period would take between 21 to 35 days, an irregular period is when you,
- menstruate frequently than the 21 days
- have abnormal uterine bleeding during period
- bleed after intercourse
- have menstrual bleeding for longer days than the usual
- bleed after your menopause
- continuous spotting during periods
The three forms of irregular periods:
“Amenorrhea”: No periods for three or more continuous menstrual cycles
“Oligomenorrhea”: Occurrence of periods for more than 35 days apart
“Menorrhagia”: Continuous bleeding that lasts a week or more
(2) Polycystic Ovaries:
The next possible sign of PCOS is the development of multiple cysts (polycystic ovaries), which occur due to the dysfunction of ovaries. Due to which the ovulation gets affected.
Ovulation takes place when a mature egg is released from the ovary to be fertilized by the sperm.
When this process fails, the egg is sent out as periods. In some cases, with women who don’t ovulate correctly, their ovaries form small fluid-filled sacs or cysts. As a result of which the ovaries fail to function regularly.
Upto 40% of infertile people with ovaries experience dysfunctional ovulation.
(3) Excess Androgen secretion:
The tiny cysts trigger the production of excess “androgens”. Androgens being the male dominating hormones, causes more problems with a woman’s menstrual cycle. Higher androgens levels may result in:
- Acne bursts in the face, neck, chest, and upper back
- Hirsutism.
- Dark patches on the skin (Acanthosis nigricans)
Some of the other symptoms include;
(4) Weight Gain:
The majority of women with PCOS experience obesity and weight gain that is hard to maintain. The reason for this is, PCOS worsens the insulin hormone that helps convert starches and sugars from the foods into energy, resulting in “insulin resistance”.
This causes insulin, sugar, and glucose build-up, leading to weight gain. Women with PCOS generally tend to carry more weight on their abdomen, which gives them an apple shape.
|
(5) Fatigue:
PCOS and fatigue are inter-connected. Most women with PCOS report increased fatigue and a dip in energy. This is due to the low vitamin B12 or vitamin D levels, hypothyroidism, and low blood count or anemia.
For women with fatigue, who still haven’t spoken to the doctor about its contributing causes, it is better to have a consultation. Similarly, underactive hypothyroidism, low vitamin B12, and anemia should also be consulted.
(6) Infertility:
PCOS could cause a delay in pregnancy, but this is not universal. But in the majority of cases, women with PCOS have infertility. While some fertility treatments are required, few others may even conceive naturally.
(7) Mood swings:
PCOS could affect mental health and impact mood swings, anxiety, and depression. A study shows that people with PCOS with low levels of serotonin and other neurotransmitters report more symptoms of depression and anxiety.
It could sometimes be associated with an increased risk of obsessive-compulsive disorder (OCD), eating disorders, and bipolar disorder.
|
(8) Pelvic pain:
Though a less common symptom of PCOS, pelvic pain may occur with periods and could combine bleeding or heavy bleeding.
(9) Headaches:
Due to the surge in hormones, PCOS could cause headaches or migraines. A 2019 study confirms that migraine is associated with PCOS. Comparatively a less common symptom, migraines could indicate PCOS if you:
- Never had them until started having other symptoms indicative of PCOS
- Have had them before but recently changes frequency and potential triggers
- When migraines are closely linked to certain phase of your menstrual cycle
(10) Sleep Problems:
PCOS could lead to poor sleep or insomnia. Of the many factors that could affect sleep, the most common one associated with PCOS is “sleep apnea”. A serious sleep disorder is when people repeatedly stop and start breathing while they sleep. This way of sleeping can never be restful and can result in depression.
(11) Depression:
Due to hormonal changes and its line of symptoms including unwanted hair growth, hair baldness can negatively affect your emotions, resulting in depression and anxiety.
PCOS risks - Is PCOS so serious?
PCOS risks in the mother-to-be
Generally, women who fall between the age group of 15 and 44 are affected by PCOS. They experience a higher risk for problems including;
- Take a long time to conceive
- Type 2 Diabetes
- Gestational Diabetes
- May encounter health risks during pregnancy
- Shoot up in cholesterol levels
High blood pressure - Coronary heart diseases or stroke
- Sleep apnea
- Dyslipidemia (presence of “bad” cholesterol, which, when uncontrolled, could lead to adverse dangerous cardiovascular outcomes)
- Increased risk of endometrial cancer
PCOS risks in pregnant women
Women who conceive with PCOS can become exposed to an increased risk of complications.
- Preeclampsia is one, which is a severe condition for both mother and baby-to-be born. Your doctor might discuss the risk factors of it and may suggest you go for a timed delivery, based on the symptom’s severity and your baby’s gestational age. Those who develop preeclampsia during your pregnancy, need careful monitoring closely
- Pregnancy-related hypertension or high blood pressure
- Gestational diabetes. This could lead you to conceive a larger baby than the average, which could lead to problems during the delivery time. The most common problem is “shoulder dystocia”, a state when the baby’s shoulder is stuck during labor time.
The PCOS-related symptoms during pregnancy can be managed with a doctor’s advice. Similarly, if you evolve gestational diabetes, your insulin level has to be in control.
PCOS risks on baby
If you develop during pregnancy, it might make things more complicated. The potential risks of PCOS on the baby are;
- Miscarriage
- Premature birth
- Large for gestational age
- Lower Apgar score
Did you know?
If you conceive a baby girl and if you have PCOS, researchers have proved that the infant might have a 50 percent chance of having PCOS.
According to an analysis of NHS data carried out by a team at Cambridge University’s Autism Research Centre, women with Polycystic Ovary Syndrome (PCOS) are likely to deliver Autistic children.
Getting pregnant with PCOS
Sometimes women may not realize they have PCOS until they fail to conceive naturally for months to years. This is because most of the time PCOS goes unnoticed.
You can get pregnant with PCOS, you need to consult your doctor about treatment.
The connection between PCOS and fertility
PCOS affects natural conception to a large extent. There are two factors by which PCOS could trigger infertility.
1. PCOS and Ovulation: It affects the natural conception by obstructing the release of eggs from the ovary, which happens customarily every month.
This might sound simple, but this could lead to a chain of other complications including irregular menstruation, which reduces the chances of ovulation.
To know more about Ovulation, check out a detailed blog written on it.
2. Another factor that could cause fertility problems is obesity. Since PCOS women put on excess weight, it could make it difficult for them to conceive.
A study points out that 60 percent of PCOS women were often obese and around 14 percent of the required proper diagnosis to get pregnant.
In contrast to the above claim, a number of myths still prevail that women with PCOS cannot conceive naturally, but the truth is, PCOS is highly treatable and most women with PCOS have chances to conceive.
Sometimes a little tweak in their lifestyle and modest weight loss could increase the chances of fertility. Few others may find it successful with basic fertility treatments and regular medications.
The hormones related to PCOS
Most often, the following hormone levels are related to PCOS. These are measured in detail during the PCOS diagnosis:
- Follicle-stimulating hormone (FSH)
- Luteinizing hormone (LH)
- Total and Free Testosterone
- Prolactin
- Dehydroepiandrosterone sulfate (DHEAS)
- Progesterone.
- Androstenedione
- Thyroid-stimulating hormone (TSH)
- Estrogen
Can PCOS lead to other chronic diseases?
Here are some of the chronic diseases associated with PCOS;
Dyslipidemia:
A metabolic condition where women with polycystic ovarian syndrome suffer from “bad” cholesterol or high LDL levels, which when left uncontrolled, could lead to adverse cardiovascular outcomes.
Hyperinsulinemia:
Women with PCOS are prone to hyperinsulinemia, which is nothing but having exceptionally high levels of insulin in the blood, which causes the liver to secrete more lipids, resulting in risky heart diseases.
Insulin Resistance:
Insulin is believed to be an appetite stimulant that can make women with PCOS crave sugary items, which can further lead to high glucose levels in the blood, worsening diabetes, and associated complications.
Pre Diabetes:
This condition increases type 2 diabetes and other metabolic conditions. Those who are recognized for type-2 diabetes should regularly follow up with their doctor to ensure their sugar levels are intact.
Coronary Heart Disease:
Women with PCOS are exposed to “atherosclerosis”, a plaque deposit in the arteries. This increases the risk of coronary heart disease and stroke.
Risk for Endometrial Cancer:
The risk of Endometrial cancer is three times more in a PCOS woman than in others. The irregular periods, the lack of periods, can lead to endometrial cancer, leading to cancer.
Having PCOS doesn’t mean you do not develop any other symptoms. It may lead you to other lines of symptoms that could be life-threatening.
It is therefore essential you stay alert on your PCOS level, switch to a healthy lifestyle, take medications as advised, and follow a healthy diet to reduce the risks mentioned above. Prevention is always better than cure!
Identifying PCOS
In a complex condition with numerous symptoms, identifying PCOS could be challenging. While some women may have a set of symptoms that could keep changing every now and then, others may not have most of them. The symptoms could be grouped into three main areas they mainly affect;
- fertility and reproductive health
- metabolic health
- psychological health
PCOS Screening
PCOS diagnosis could be a challenging diagnosis for any physician to make. To classify it as a syndrome, a constellation of symptoms has to be scrutinized, including signs of hyperandrogenism, infertility, amenorrhea, acne, hirsutism, etc.
Also, there is no single test to diagnose it or a fool-proof algorithm that the physicians could use to assess patients. The diagnosis can be especially challenging in adolescents or perimenopausal or menopausal women and in early teens.
Contacting a fetal expert, obstetrician, or gynecologist can help with effective diagnosis. To start with, she would understand three characteristic features of polycystic ovary syndrome including;
- Anovulation
- High levels of androgens
- Cysts on the ovaries
Possessing one or more of the above features could lead to PCOS diagnosis. On arriving at a conclusion, your obstetrician – gynecologist will rule out other conditions that might have similar PCOS symptoms including;
- Thyroid dysfunctions
- Excess hormone secretion by the “adrenal hyperplasia”
- Excess hormone secretion is called “hyperprolactinemia” by the hormone prolactin in the pituitary gland.
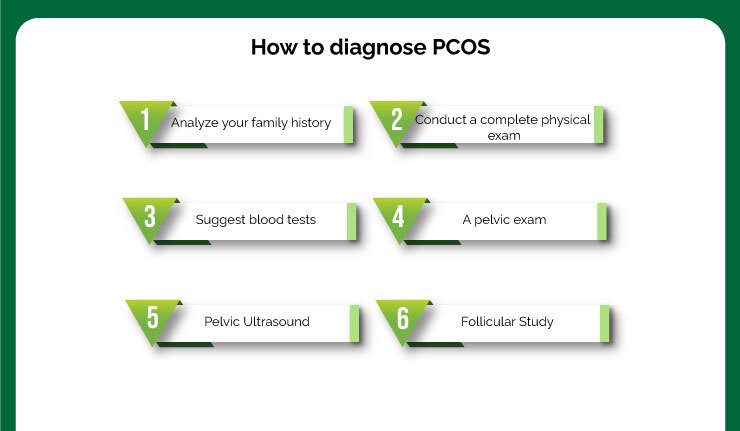
PCOS Diagnosis
1. Analyze your family history:
Your doctor may try to study all signs and symptoms you’ve noticed in your body. As this is a crucial step, she will figure out your medical history, lifestyle, including your menstrual periods and weight changes.
If you have been having irregular periods, she might try to ponder further to understand your puberty history, developmental delays, your sleep, and dietary patterns, anxiety, and stress levels, exercise, and other lifestyle habits, etc.
There are chances for PCOS to run in families. Your doctor will hence try to understand whether your mother or sister has had PCOS syndrome or has faced difficulty getting pregnant.
2. Conduct a complete physical exam:
Your doctor will examine you physically to understand more. She will check you for signs of hair growth, insulin resistance, acne, dark patches, and other visual signs to understand androgen levels.
The doctor could check your blood pressure test, measure up your waist, and assess your body mass index.
3. Suggest blood tests:
A very small amount of blood sample is drawn from a vein in your arm to analyze the following hormone levels.
- Follicle-Stimulating Hormone (FSH) which affects women from getting pregnant is measured. If you have PCOS, the FSH level is usually normal or lower than normal
- Estrogen is a stimulating hormone that induces periods in women. Depending on whether or not you have PCOS, your level may be high or normal
- Testosterone, the sex hormone measures more if you have PCOS
- Luteinizing hormone (LH) which is medically proven to revive ovulation is measured
- Sex Hormone Binding Globulin’s (SHBG) level may be lower than normal if you have PCOS
- Androstenedione, again a sex hormone called may be higher-than-normal if you have PCOS in you
- Human chorionic gonadotropin (hCG) hormone test is used to check if you are pregnant
- Anti-Mullerian hormone (AMH) is used to examine how well your ovaries are working and to estimate when your menopause approaches. The AMH level is higher with PCOS.
A few other tests may be recommended to rule out conditions like tumors, thyroid problems, and hyperplasia (a condition of organ-swelling due to cell accumulation) that has similar PCOS symptoms.
4. A pelvic exam:
Following the above tests, your doctor will then visually and manually inspect your reproductive organs to examine if there are any growths, masses, or any other abnormalities through a pelvic study. She inspects the shape, size, and position of the uterus and ovaries. The vagina, fallopian tube, cervix, and rectum are also checked.
5. Pelvic Ultrasound:
To understand if you have cysts in your ovaries, your doctor might recommend an ultrasound. This is used to give a clearer picture of your pelvic area using the sound waves. She will concentrate on checking the lining of your uterus, which is usually thicker if you have irregular periods.
When you have PCOS, your ovaries may be 1½ – 3 times thicker and larger than normal. The pelvic ultrasound validates ovarian changes in about 90 percent of women who have PCOS.
6. Follicular Study:
A follicular study is used to ascertain the size of any active follicles in the ovaries which can contain an egg. To a couple that is trying to come through fertility treatment, this line of scans helps determine the presence of follicles and the best time to extract an egg for fertilization.
It is also used to effectively predict ovulation so that fertilization happens naturally. The couple can have intercourse during those specific ovulation times to increase their chances of pregnancy.
Post-diagnosis Tests:
On confirming PCOS, additional tests including the following could be suggested to understand your overall health conditions;
- Periodic checks of glucose, cholesterol, blood pressure, glucose tolerance, and triglyceride levels are suggested
- Screening for depression and anxiety
- Screening for obstructive sleep apnea
- Lipid profiles check is done to check your triglycerides and cholesterol levels because often PCOS could develop heart diseases.
- To test diabetes, a glucose test is done. This is again a majority of women with PCOS are prone to diabetes.
- Insulin resistance is conducted to study how your body responds to insulin that helps arrest blood sugar levels. When it is proven that your body doesn’t respond to the insulin secreted, then you may have insulin resistance. This is very common with PCOS women and could lead to diabetes.
PCOS Medications
The first point of focus of your doctor is to regulate your menstrual cycle. Based on the diagnosis she might recommend personalized medication which might include some of them below.
Combination pills (birth control):
Usually oral contraceptives contain estrogen and progestin, the artificial versions of female hormones that are naturally produced in the ovaries. A combination of these birth control pills compress androgen production, regular estrogen, and keep your ovaries from releasing an egg.
Progestin therapy:
Taking a progestin as per the doctor’s advice regulates your periods and protects against endometrial cancer. It lets other hormones function well.
Progestins prevent anemia and menstrual blood loss. They could be available in the form of tablets, suspensions, gel/jelly, capsules, or suppositories.
Depending on the dosage of consumption, progestin can have different results.
While high doses of progesterone are ideally suggested for women to continue their pregnancy, low doses are recommended to prevent pregnancy from occurring.
Some of the other benefits of progestins are:
- Regulates the menstrual cycle and treats “Amenorrhea”, the unusual stopping of the menstrual periods.
- Helps boost progesterone level in the body
- It prevents the estrogen from thickening the lining of the uterus
- Treats endometriosis condition, where unusual heavy bleeding of the uterus starts or stops the menstrual cycle
Some other effects of Progestin could have effects like weight gain, hike in body temperature, progression of glands for milk production and breastfeeding, relaxing the uterus to sustain a pregnancy.
Vitamin Supplements:
Your doctor might suggest supplements that can help alleviate PCOS-related ailments.
- Inositol, a Vitamin B supplement to boost insulin resistance. Chromium to improve your BMI, that’s a prerequisite for PCOS. This also stabilizes insulin resistance in your body.
- Cinnamon extract is believed to have a positive impact on insulin resistance. It even is said to regulate menstruation for women with PCOS.
- Turmeric decreases insulin resistance and acts as an anti-inflammatory agent.
- Zinc boosts your total immune system and improves fertility. It also controls excessive unwanted hair growth in your body
- While vitamin D acts as vital to your endocrine system
Supplements for Ovulation
To boost ovulation, your doctor might recommend supplements including:
- Letrozole (Femara): A breast cancer treatment, this is sometimes used to stimulate the ovaries.
- Clomiphene: An anti-estrogen medication, which induces ovulation, is often suggested to be taken during the first part of your menstrual cycle.
- Gonadotropins: The hormonal medications usually injected, encourages ovarian functions.
- Metformin: An oral medication, this is used for Type 2 diabetes. The metformin lowers insulin levels and improves insulin resistance. Usually, when Clomiphene doesn’t work, doctors prefer adding metformin to the medication. To those with prediabetes, Metformin can block type 2 diabetes and can help in weight loss.
Supplements for excessive hair growth:
Birth control pills: Prescribed to decrease androgen production in your body that triggers unwanted hair growth.
Spironolactone: Otherwise referred to as Aldactone, this medication stops the progression of androgen side effects on the skin.
Caution has to be taken here because Spironolactone can cause birth defects, therefore, effective contraception is essential during its intake.
Word of caution – this is recommended only when you are planning to become pregnant or if you’re pregnant.Eflornithine (Vaniqa): This facial cream can slow facial hair growth.
Electrolysis: A process by which a tiny needle emitting an electric current is inserted into each hair follicle to damage and in the due course, destroys the follicle.
PCOS tips and treatment - What can women with PCOS do to conceive naturally?
Though sometimes the time taken for the PCOS treatment is long, it is proven that women with PCOS actually end up having the same number of children like other women.
Here are some ways by which you can try increasing your chances of becoming pregnant with PCOS.
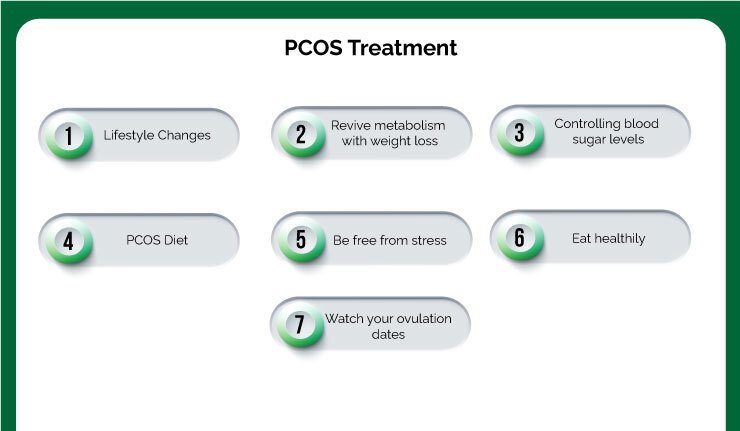
Lifestyle Changes:
The first line of treatment that’s recommended for women with PCOS is certain lifestyle changes including diet, weight loss, and exercise.
If you are overweight, your doctor may recommend a weight loss regime with a low-calorie diet with a mix of some moderate exercises.
Revive metabolism with weight loss:
Obesity substantially contributes to metabolic and reproductive abnormalities in PCOS. Fighting weight loss boosts the chances of getting pregnant.
The extra weight in you could lead to unwanted stress and inflammation. Maintaining BMI can regularize menstruation. Even if it’s shedding five percent from the total weight, it improves the chances of conceiving naturally in PCOS women.
Therefore try indulging in regular physical activity like walking, weight lifting, cardio, and exercises to counter stress and keep fat under control.
While exercising, be mindful to reduce your abdominal fat. Cycling can boost your metabolism and helps in losing abdominal fat.
PCOS Diet
Consume more anti-inflammatory foods:
To ease PCOS-related symptoms consume more tomatoes, leafy greens, olive oil, fish variety like tuna, mackerel, nuts to fight inflammation. You could also try;
- To evenly space out carb-rich foods throughout the day
- To avoid beverages and sugary foods
- Fill half your plate with veggies
- Eat more fruits
- Consume beans, legumes, and unsaturated sources of fat
- Consider having more iron-rich foods including eggs, broccoli, spinach.
- Boost your magnesium-rich intake with almonds, bananas, cashews.
- Intake more fiber to improve your digestion including lentils, brussels sprouts, lima beans, pears, and avocados
- Cut down on coffee and increase with a decaf alternative like herbal tea.
- Have more red meat, beans, seafood to boost zinc intake and to improve irregular periods and ovulation
- Cod liver oil is rich in Vitamin A & D, and omega-3 fatty acids, which helps PCOS women menstruate regularly. It also helps get rid of the abdominal waist.
Be free from stress:
Due to the hormonal imbalances, depression and anxiety mount up in PCOS women. They could result in mood swings. Relaxation is the only remedy. Try simple yoga poses that could ease tension, calm, stress, and improve blood sugar levels. Just sitting in a quiet, comfortable spot, and focusing on your breath could help too.
Eat healthily:
You won’t be successful if you just exercise or meditate. A combination of a healthy diet plan plays a major role in helping those who are struggling to conceive with PCOS. Follow a low-carb diet with lots of proteins, nuts and seeds, and foods rich in vitamins like B12, iron, D, folate, iron, omega-3, which act as natural fertility boosters.
Controlling blood sugar levels:
Insulin resistance can trigger diabetes, which directly impacts conception. Therefore trying to control blood sugar levels may bring a change in reproductive health.
Watch your ovulation dates:
Keep track of your ovulation dates either by maintaining a record-keeping or with the help of an ovulation app. Alternatively, try using Ovulation Kit from the pharmacy store to know on which days you are most fertile for sexual intercourse.
Why is PCOS more common in India these days?
The PCOS Society states that out of one in every 10 Indian women in India has polycystic ovary syndrome (PCOS), and six out of 10 diagnosed women were teenage girls.
A startling nationwide survey by the Indian Council of Medical Research (ICMR) proves the severity of the syndrome that it can turn dangerous if left unchecked, and could lead to irrevocable infertility, along with another line of long-term health effects.
Though PCOS has been in India for very long, people still lack awareness about PCOS, and it remains undetected in many. In fact, it is this lack of consciousness that affects nearly around 10 million women, across the world.
According to the study by AIIMS by its department of endocrinology and metabolism, roughly around 20 to 25% of Indian women suffer PCOS at their reproductive age.
The results proved that the symptoms of Indian women had been mixed; the results confirm that while 35-50 percent of women had fatty liver, 60 percent of women were obese with androgen hikes, and 70 percent had insulin resistance.
Early intervention and treatment is the only key to prevent PCOS related health problems.
Questions To Ask Your Doctor About PCOS
It is hard to manage PCOS. Learning that you have the syndrome can be daunting as the implications can travel throughout your reproductive years, affect your hormone levels, and your general health.
Be open with your doctor. Discuss questions that you need to be sure of. The 10 Most commonly asked questions about PCOS are here in this blog, read it for clarity.
Conclusion:
PCOS can disrupt women’s hormones and make it difficult to get pregnant. What’s necessary is a positive attitude towards your body and early intervention with the help of your doctor or a fetal expert.
Grow more aware of the changes in your body and overcome PCOS with the right diagnosis. Stay calm for the next big days to follow.
Chennai Women’s Clinic is now Jammi Scans
Deepthi
Dr. Deepthi Jammi (Director, Jammi Scans) is a qualified OB/GYN and Post-Doc in Maternal Fetal Medicine. As a pregnancy ultrasound expert, she is passionate about healthy pregnancies and works towards spreading awareness on the latest diagnostic options available for parents to choose from. Dr.Deepthi has received gold medals and awards in Fetal Medicine at international and national conferences, and has appeared in numerous prestigious regional magazines and TV interviews.